- ESKAPE-E refers to a group of clinically significant, highly antibiotic-resistant bacterial pathogens: Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, Enterobacter spp., and Escherichia coli.
- Antimicrobial resistance (AMR), including extended-spectrum β-lactamase (ESBL) and AmpC resistance in ESKAPE-E pathogens is recognized as a leading global public health threat.
- While AMR is often associated with hospitals and clinical environments, fresh produce can also act as a vehicle for transmitting multidrug-resistant (MDR) bacteria.
- In South Africa, smallholder farms are critical for food security. Understanding environmental reservoirs of AMR in these systems is essential for designing interventions to reduce transmission from farm to consumer
Key findings: Viviers et al. tested 224 samples (44 irrigation water, 85 soil, 95 fresh produce) collected from six smallholder farms in South Africa. The following outcomes were reported1:
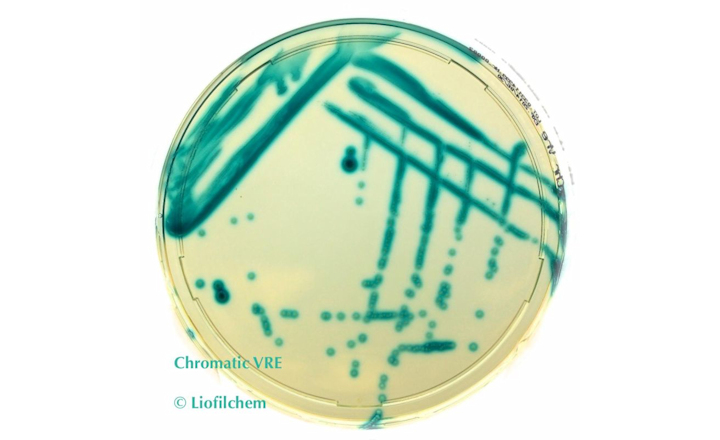
- Prevalence: ESBL/AmpC producers were detected in 17% of samples (38/224).
- Resistance profile: Of the isolates, 47% were ESBL-producers and 43% AmpC-producers.
- Enterobacterales isolates showed resistance to aminoglycosides, penicillins, and glycylcyclines, with highest resistance to fluoroquinolones (97%), macrolides (94%), quinolones (92%), and cephalosporins (92%).
- Isolates:
- 35 Enterobacterale strains were isolated, including Enterobacter spp. (26%), Klebsiella spp. (26%), Serratia spp. (17%), E. coli (9%), Proteus spp. (6%), Citrobacter spp. (6%), Leclercia spp. (6%), Salmonella enterica (3%). Most were collected from fresh produce (19/35, 54%), followed by soil (11/35, 31%) and water (5/35, 15%).
- 15 P. aeruginosa strains were isolated, including from fresh produce (8/15, 53%), water (5/15, 33%) and soil (2/15, 14%).
- Environmental sources:
- Water: highest prevalence in borehole and river samples, followed by municipal and dam water.
- Soil: higher prevalence in fields fertilized with animal manure compared to organic compost.
Bigger picture: Across Europe, antimicrobial-resistant bacteria are responsible for more than 800,000 infections and 35,000 deaths each year.2 A review by Denissen et al. (2022) highlighted the persistence of ESKAPEE pathogens beyond clinical settings—appearing in water, soil, and food.3 Yet, data from informal farming systems remain sparse, where monitoring and regulatory oversight are limited.
The findings of Viviers et al. underscore the presence of clinically significant MDR Enterobacterales and P. aeruginosa in smallholder farm environments.1 These results emphasize a growing need for stronger surveillance systems, targeted interventions, and comprehensive risk assessments across the water–soil–plant nexus to limit the spread of AMR into the food chain.
References:
- Viviers et al. 2025. “Occurrence and Genotypic Characterization of Selected Multidrug-resistant ESKAPE-E Pathogens Isolated from Integrated Smallholder Fresh Produce Farms.” Journal of Food Protection. Vol. 88, Issue 7, page 100543.
- European Centre for Disease Prevention and Control (ECDC) (2022). Assessing the health burden of infections with antibiotic-resistant bacteria in the EU/EEA, 2016–2020. Accessed on October 2, 2025 from
- Denissen et al. 2022. “Prevalence of ESKAPE pathogens in the environment: Antibiotic resistance status, community-acquired infection and risk to human health.” International Journal of Hygiene and Environmental Health. Vol. 244, page 114006.