Why This Matters:
- Gram-negative bacteremia caused by resistant pathogens (e.g., ESBL-producers, carbapenemase-producers) is associated with significant morbidity, mortality, and cost.
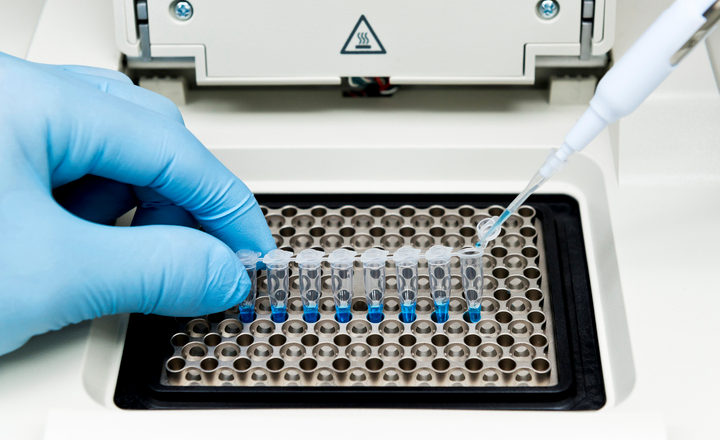
- Traditional phenotypic antimicrobial susceptibility testing (AST) requires isolate growth and may delay resistance information by 24-48 hours or more. A direct multiplex PCR from positive cultures potentially shortens turn-around time.
- Faster knowledge of resistance determinants supports antimicrobial stewardship, enables earlier optimal therapy, and may reduce empirical broad-spectrum use and resultant selection pressure.
Key Findings: Marxreiter et al. (2025) used 148 blood cultures that were positive for Gram-negative bacteremia to assess a multiplex PCR panel (BIOFIRE FILMARRAY) that detects 31 different antimicrobial resistance (AMR) genes and compared its performance against phenotypic AST (broth microdilution).1
- The panel detected a large menu of resistance genes (for example, major β-lactamase genes, carbapenemases) directly from culture broth, demonstrating feasibility of the direct-from-blood approach.
- Results showed good alignment between gene detection and phenotypic resistance for many but not all antibiotic-gene combinations — underscoring that gene presence ≠ always phenotypic resistance, and gene absence ≠ susceptibility.
- Sensitivity for predicting antimicrobial resistance was ≥90% for E. coli and K. pneumoniae.
- However, sensitivity for predicting antimicrobial resistance was poor for P. aeruginosa, Enterobacter cloacae complex, and Acinetobacter baumannii.
- Simulated stewardship for E. coli or K. pneumoniae bloodstream infections resulted in significant de-escalations to narrower a narrower-spectrum agent.
- Turn-around time was significantly reduced compared to traditional workflows, enabling earlier availability of resistance information.
Bigger Picture: This work contributes to the evolution of rapid diagnostic stewardship in bloodstream infection management — moving from pathogen identification alone to early resistance-mechanism detection. For clinical microbiology labs and antimicrobial stewardship programs, deploying multiplex PCR directly on positive blood cultures offers a path to earlier optimization of therapy, potentially improving outcomes and reducing resistance selection. However, molecular alone is not a complete answer — integrative strategies combining rapid diagnostics, phenotypic AST confirmation, stewardship protocols, and real-time clinical action will define the impact. In the era of rising Gram-negative resistance, this approach will be a key component of future diagnostic workflows.
Reference:
- Marxreiter et al. (2025). Rapid detection of gram-negative antimicrobial resistance determinants directly from positive blood culture broths using a multiplex PCR system. Journal of Clinical Microbiology, e0038425.
(Image Credit: iStock/unoL)