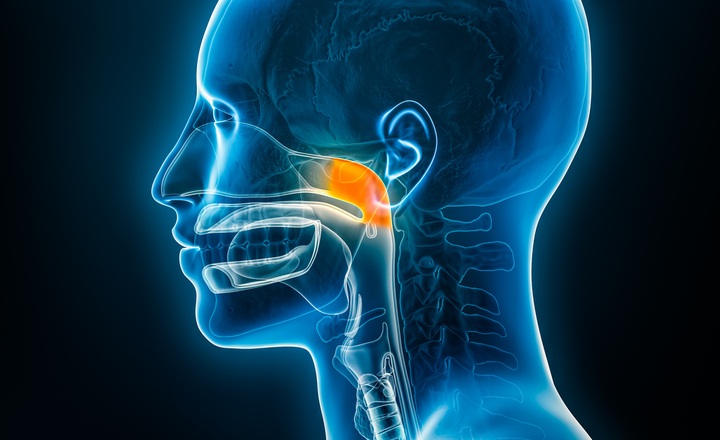
- Recurrent acute otitis media (rAOM) is a common pediatric condition, particularly in children under 3 years of age, with high healthcare utilization and frequent antibiotic prescriptions.
- The nasopharyngeal microbiome plays a central role in susceptibility, pathogen carriage, and disease recurrence, yet longitudinal dynamics in real-world pediatric populations are poorly understood.
- Insights into how age and antibiotic exposure influence microbial community structure can inform prevention, stewardship, and therapeutic strategies.
Key Findings:
Van Dongen et al. (2025) conducted longitudinal nasopharyngeal sampling in 58 children aged 6–25 months with a prior diagnosis of recurrent acute otitis media (rAOM) to assess, using 16S rRNA gene sequencing, how age and antibiotic exposure shape upper respiratory microbiome dynamics over.¹
- Age-dependent microbiome maturation: Older children exhibited a lower incidence of AOM, reduced otopathogen burden, and increased relative abundance of Moraxella spp. and other commensal taxa compared with younger children, consistent with progressive maturation of nasopharyngeal microbial communities that may confer protection over time.
- Protective taxa associated with antibiotic-free intervals: Higher relative abundances of Corynebacterium, Dolosigranulum, and Moraxella positively correlated with the number of antibiotic-free days preceding sample collection.
- Antibiotic exposure disrupts community structure: Recent antibiotic use was associated with reduced microbial diversity and increased dominance of opportunistic taxa, including potential otopathogens such as Streptococcus, Pseudomonas, and Haemophilus.
- Microbiome instability and disease recurrence: Children experiencing multiple recent AOM episodes demonstrated greater temporal fluctuation in microbiome composition compared with children with fewer episodes, indicating reduced community stability.
- Otopathogen persistence patterns: Key rAOM-associated pathogens, including Haemophilus influenzae and Streptococcus pneumoniae, were significantly more prevalent in samples collected during AOM episodes than during AOM-free visits (S. pneumoniae: 92.6% vs 76.9%, P = 0.013; H. influenzae: 60.0% vs 43.4%, P = 0.021), and were more frequently detected following antibiotic exposure and in children with higher recurrence rates.
Bigger Picture: This longitudinal analysis highlights the dynamic interplay between host age, antibiotic exposure, and the upper respiratory microbiome in children prone to recurrent acute otitis media. The findings support the concept that microbiome maturity may confer resilience to perturbation, while antibiotic use — especially repeated courses — disrupts microbial equilibrium and may contribute to pathogen persistence and disease recurrence. For clinicians and stewardship programs, these data underscore the importance of judicious antibiotic prescribing and consideration of age-specific microbiome development when managing rAOM. Further research into microbiome-modulating interventions may offer new avenues for prevention and durable disease control.
(Image Credit: iStock/libre de droit)
References:
- Van Dongen et al. (2025). Age and Antibiotic Use Influence Longitudinal Dynamics of the Upper RespiratoryMicrobiome in Children with Recurrent Acute Otitis Media. mSphere.