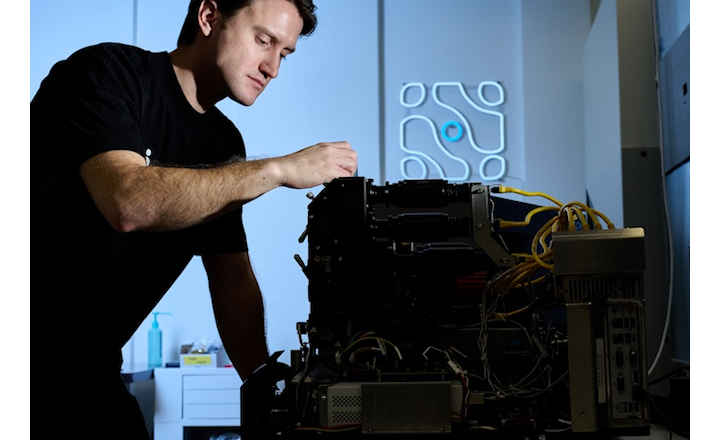
Why This Matters:
- Medicinal products must meet strict microbiological purity and sterility standards to protect patient safety.
- Outbreaks and contamination events — ranging from endotoxin or fungal contamination in compounded injectables to bacteria in oral syrups — demonstrate that current QA systems can fail.
- Understanding contamination sources, regulatory frameworks, and preventive strategies is essential for manufacturers, regulators, and healthcare providers.
Key Findings:
Tyski et al. (2025) has reviewed historical and recent evidence on microbiological contamination of medicinal products, regulatory requirements, pharmacopoeial testing frameworks, and documented case reports of contamination and recalls.1
Regulatory expectations: Pharmaceutical products must either be sterile or comply with applicable microbiological purity criteria in pharmacopoeial monographs; sterility is mandatory for parenteral, ophthalmic, and high-risk products, while non-sterile products follow microbial limit tests.
Real-world contamination incidents: Historical outbreaks — such as contaminated vaccines (1902), intravenous fluids linked to Enterobacter cloacae and Pantoea agglomerans, and the 2012–13 fungal meningitis epidemic — illustrate the severe consequences of contaminated medicinal products.
Diverse microbial threats: Isolated contaminants include Gram-negative and Gram-positive bacteria, anaerobes, yeasts, and moulds, as well as extracellular toxins (e.g., endotoxins, mycotoxins), which can cause drug deterioration, pyrogenicity, or patient harm even in the absence of live organisms.
Challenges in non-sterile products and raw materials: Water-based formulations, herbal products, and raw materials of plant or animal origin are especially prone to microbial contamination, with opportunistic pathogens like Burkholderia cepacia complex frequently implicated in recalls and outbreaks.
Pharmacopoeial harmonization and testing: Harmonized monographs from major pharmacopoeias (Ph. Eur., USP, JP) outline standardized sterility and microbial limit tests, yet gaps remain in detecting non-cellular contaminants (e.g., prions, viruses) and in addressing contamination introduced during compounding or dispensing.
Bigger Picture:
Microbiological contamination of medicinal products encompasses a spectrum of quality and safety issues — from sterility failures and substandard hygiene in manufacturing to contaminated raw materials and lapses during compounding or storage. While adherence to Good Manufacturing Practice (GMP), robust quality systems, and pharmacopoeial testing substantially reduce risk, documented contamination events and product recalls underscore that risks persist. Vigilance through rigorous environmental controls, comprehensive microbial monitoring, pharmacopoeial compliance, and post-market surveillance remains essential to ensure medicinal products are safe and effective.
(Image Credit: iStock/ AscentXmedia)
References:
- Tyski et al. (2025). Microbiological Contamination of Medicinal Products — Is It a Significant Problem? Pharmaceuticals.