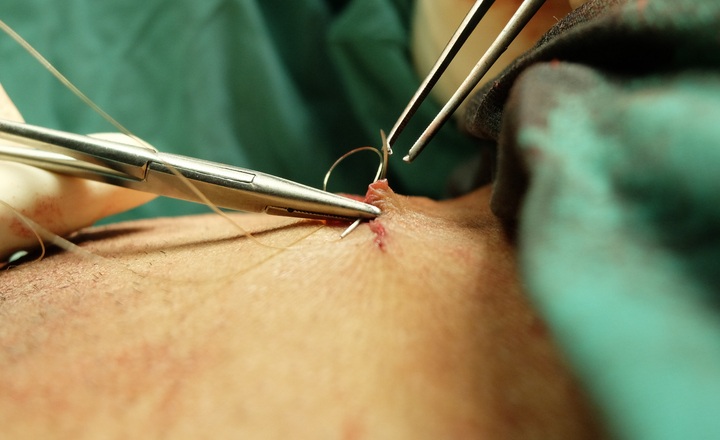
Why This Matters:
- Surgical site infections (SSIs) are among the most frequent healthcare-associated infections: They increase morbidity, prolong hospital stays, and substantially raise healthcare costs.
- Microbial resistance complicates management: Knowledge of prevalent pathogens and their resistance patterns is essential to improving empirical therapy, tailoring prophylaxis, and reducing postoperative infection burden.
- Surgical specialties differ in microbiology: Abdominal and neurosurgical wounds have distinct microbial ecosystems; characterizing this aids targeted antimicrobial stewardship and better patient outcomes.
Key Findings: Agrawal et al. conducted a prospective study at a tertiary care hospital in Central India involving 78 patients who developed clinically diagnosed surgical site infections (SSIs) following laparotomy or neurosurgery.1
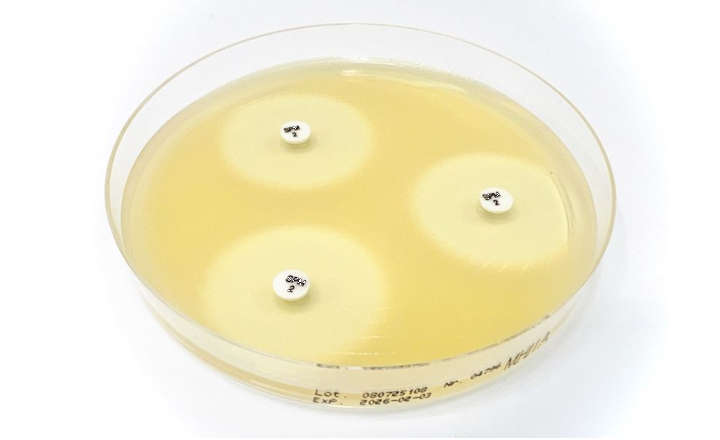
- Incidence and Culture Positivity: 62.8% of cases yielded positive cultures.
- Predominant Pathogens: Escherichia coli was the most commonly isolated (~22%), followed by Staphylococcus aureus (~19%) and Pseudomonas spp. (~9%)
- Antimicrobial Susceptibility Patterns: E. coli showed high resistance to (~83%) to cefoxitin, ciprofloxacin (~53%), ceftriaxone (~59%) and amikacin (~47%). For S. aureus isolates, ~40% were resistant to clindamycin and ciprofloxacin. For Pseudomonas spp., ~86% were resistant to ciprofloxacin, ~72% were resistant to amikacin and ~57% were resistant to ceftriaxone and piperacillin + tazobactam
- Concomitant Infections: In patients with surgical site infections (SSI) AND concomitant infections, E. coli was most frequently associated with urinary tract infections (18% of cases), whereas SSIs involving S. aureus were mainly linked with bloodstream infections (15% of cases).
Bigger Picture: For surgeons and infection control teams, this study underscores the importance of site-specific empirical therapy guided by local resistance patterns, particularly given the high rates of multidrug-resistant E. coli, Pseudomonas spp., and S. aureus.
Early identification of pathogens, combined with vigilant postoperative monitoring and strict adherence to aseptic techniques, can reduce the incidence of SSI. Integrating antimicrobial stewardship with comprehensive infection prevention - especially in high-risk procedures such as laparotomy and neurosurgery - remains essential to improving outcomes and limiting the spread of resistant organisms.
The findings also demonstrate the interconnectedness of infection sources, as SSIs frequently co-occur with urinary tract or bloodstream infections, suggesting that comprehensive surveillance and integrated infection prevention strategies are necessary to limit pathogen spread.
Overall, the study reinforces that tailored antimicrobial stewardship, vigilant postoperative monitoring, and adherence to aseptic surgical protocols are key to reducing SSI rates, improving patient outcomes, and combating the spread of multidrug-resistant organisms in high-risk surgical populations.
(Image Credit: iStock/ EyeEm Mobile GmbH)