Why this matters:
- There is increasing demand for product sterility testing in clinical microbiology laboratories due to the rapid development of cellular-, gene-, and immuno-therapies.
- Sterility testing ensures that biologics and pharmaceutical preparations are free from microbial contamination, preventing potentially life-threatening adverse events.
- Regulatory oversight differs substantially between clinical and cGMP testing laboratories, with the former falling under CLIA/CAP and regulated by the CMS and the latter falling under FD&C Act and regulated by the FDA, which have different and unique requirements for quality systems and laboratory practices.
- Notably, implementation of cGMP is expected for Phase I clinical trials and increases as the product matures toward commercialization, placing increased sterility testing demands on clinical microbiology laboratories.
Key Findings: The authors emphasize the following points for clinical microbiology laboratories:
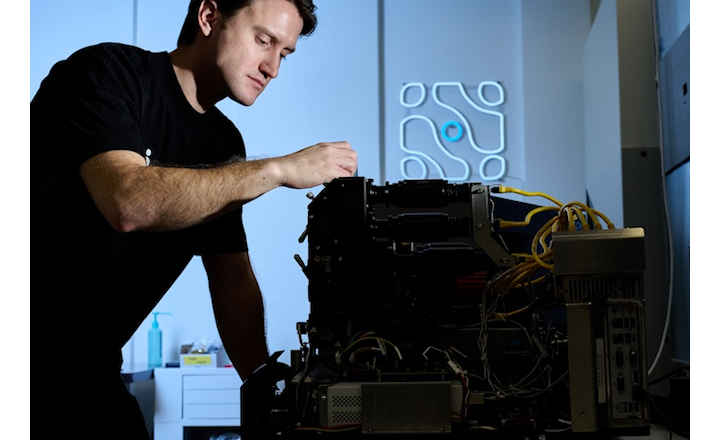
- A robust quality management system is the backbone of cGMP programs; central to cGMP is validation of equipment, software, and systems through installation, operational, and performance qualification (IQ, OQ, and PQ).
- Nuanced differences between the CAP and IQ, OQ, and PQ regulatory requirements are outlined and the IQ, OQ, and PQ framework is applied to case studies involving blood culture systems, controlled temperature units, and LIMS.
- Recommendations include:
- Risk-based approach: focusing validation efforts on instruments most likely to affect sterility results.
- Quality control integration: Routine checks, calibration, and preventive maintenance are critical to maintaining a validated status.
- Training & documentation: Properly trained personnel and detailed SOPs/documentation are essential for reproducibility and regulatory inspections.
Bigger Picture: Proper equipment validation lies at the heart of sterility testing and is mandated by FDA, USP, and ISO standards. As novel therapies and biologics progress through advanced clinical trial stages, sterility testing grows increasingly complex, with heightened cGMP expectations under FDA oversight. This review offers a practical roadmap for clinical microbiology laboratories, which often operate under CLIA/CAP rather than full cGMP frameworks required by FDA. Adopting the IQ/OQ/PQ validation structure is key to achieving reliable results, regulatory compliance, and ultimately safeguarding patients while supporting clinical innovation.
Reference:
- Gebo et al. (2025). All you need to know about equipment validation for sterility testing. Journal of Clinical Microbiology. Vol. 63, Issue 9: e0147724.