There is no arguing that cell and gene therapies are the most advanced and complex drugs ever made. Developers of cell and gene therapies must contend with significant challenges in their fundamental development and manufacturing process, from the donor cell to final drug product delivery. The traditional sterility test, taking 14 days to complete, has long been a challenge to ensure patient safety while getting therapies to patients as quickly as possible. Shortening the time to result of the sterility release test has been paramount since most of these therapies are administered at risk to patients ahead of sterility test results. Between dosage and final test results, this period places patients in an unnecessarily long window of risk.
While certain rapid microbiological methods have been used in cell and gene therapy manufacturing for some time now, their application has been limited. Much of this has been due to the technologies themselves, whether from incompatibility factors with membrane filtration and direct inoculation methods, inconsistent detection of common contaminants such as molds, or limited sample compatibility among different therapeutic modalities. Even those technologies that provide continuous monitoring have demonstrated inconstant time-to-detection among industry-relevant molds or slow-growing organisms. Inconsistent time-to-detection when a product is already in a patient is counter-productive, as it still leads to an unknown at-risk period for the patient. These technological limitations should not continue to limit the industry as a whole.
Though rapid microbiological methods (RMMs) provide benefits once implemented, they should be easy to validate, operate, and expand internally, supporting rapid testing applications throughout early development to final release. Adding complexity to implementation or reducing the scope of an RMMs application is an inefficient use of time and resources, which may be better spent developing and producing more breakthrough products. An RMM should allow companies to continue striving toward improving production efficiency, data integrity, patient safety, and the medical breakthroughs that these therapies can deliver, rather than limit them.
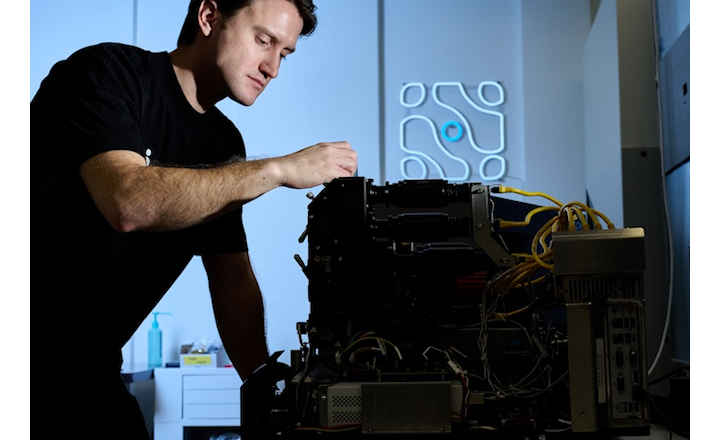
With the addition of the Celsis Adapt™ concentrator, Charles River has now expanded the capabilities of our Celsis® rapid microbial detection platform to detect contamination in products containing cells, including cellular therapies and samples also found upstream biomanufacturing. The Celsis Adapt can efficiently lyse the therapeutic cells in these products, neutralize non-microbial ATP, and remove the remaining debris while retaining bacterial, yeast, and fungal contaminations. This technology has turned other's limitations into strengths, having addressed many challenges typically faced by RMMs in the test method and sample compatibility, allowing multiple applications within a production process. Manufacturers can now adopt a confident release test for advanced medicinal therapies and short shelf-life products in as little as three days following the risk-based approach developed by the industry or between 4 and 7 days, depending on the application. These time-to-release claims also mean the accurate and consistent detection of bacteria, yeasts, and molds, including slow-growing organisms.
This product expansion further connects our QC microbial testing portfolio for advanced medicinal therapies and short shelf-life products by adding to the already existing rapid, accurate and consistent product line that the life sciences industry has trusted for decades. When a patient's at-risk period can be closed with absolute confidence within a finite period of time, we are now delivering patient treatment and patient safety at the same time.
But, at that point, you’re too late. Not only have you had a microbial contamination event, but you’ll be met with a lot of questions, and you’ll wish you answered them before the test. The PDA TR 88 report lists a variety of questions to ask when investigating your result, and almost all of them serve a better purpose when used pre-emptively. Try it out! Re-word some of the questions throughout the report to identify current gaps in your laboratory or manufacturing process for investigating microbial contamination events.
Instead of waiting until after a failing sterility test to ask:- Was all test equipment (HEPA, isolator, filtration apparatus, etc.) acceptable at the time of use
- Was there ongoing construction in the facility?
- Are the manufacturing areas, transition zones, material transfer areas, testing laboratories, etc. organized for proper flow of items?
Right now, you can ask:
- What systems do we have in place to ensure all test equipment is acceptable before use?
- What are our controls to ensure facility construction does not impact product quality?
- How can we organize areas to minimize routes of microbial introduction?
Human Factors: Always Under the Microscope
Potential for microbial introduction during sampling and testing was a common theme in the PDA TR 88 report. Not surprisingly, there are example questions to ask a technician about those tasks. Since microbial contamination results take up to two weeks to generate, memories of the sample in question can fade, especially when the tech repeats similar sample collection and testing the days before and after the event.
To limit glaring training gaps found after an event, you need to evaluate the robustness of your training program now.
Ask yourself:- Are my operators, technicians, and analysts empowered to halt a process if they identify something unusual?
- Will they feel penalized with extra hours if they follow up on something unusual?
- Does management’s emphasis on completing a test detract from an analyst’s attention to do it correctly?
If you do not have a good handle on these items prior to a micro event, you could find multiple routes of microbial contamination during your investigation. It’s unlikely they all played a role, yet you’ll need to chase down impact and corrective actions for every gap you identify. If you don’t, inspectors reading your reports will undoubtedly have more intense questions for you.
If you do have a good handle on these items prior to a micro event, your investigation scope can focus on the most likely contributors.
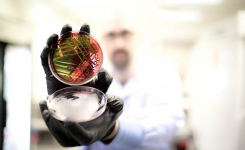
Environmental monitoring is essential in microbial contamination investigationsRoot cause confirmation depends almost entirely on a microbial identification that aligns your discrepant result with a contamination source. It’s best practice to trend your recoveries and identifications . Microbial contamination investigations move quickly when you know where you’ve seen the organism before, as opposed to sampling investigative locations after the fact. When you recover an out-of-trend result with your product you can easily review the most likely contributor. It could be a specific area, utility, or raw material.
It’s also possible you found a very common organism in your product, like S. epidermidis. That organism is so common you may have seen it in raw materials and multiple environmental samples. As you investigate those sources, you can further compare organisms with strain typing to pinpoint a definitive source.
As outlined in the PDA TR 88 report, the systems that generate microbial IDs cannot be taken for granted. Small changes in sample prep can lead to varying IDs. Organisms missing from a system library can result in a non-ID, or worse, a match to the next closest thing. You must be confident your system generates the same result when you repeatedly challenge with the same organism. A Roseomonas by any other name will send you looking elsewhere for the root cause.
Knowing your microbiota prior to a microbial contamination event is emphasized in another recently released report, the FDA Guidance for Non-Sterile products released in 2021. The guidance addressed some product recall case studies. Root causes were almost impossible to verify because sites had poor historical data from their manufacturing environment. Recommendations for proactive facility monitoring are more than just a trend with regulators and industry thought leaders.
Learn more about the Celsis Adapt here or contact the supplier for details using the green request information button below.