Why This Matters:
- PRP contamination poses clinical risks: Platelet-Rich Plasma (PRP) is commonly used in regenerative medicine. PRP can be contaminated during collection and preparation, potentially causing post-procedural infections.
- Rapid detection gaps: PRP is typically administered shortly after preparation; conventional sterility tests take too long, leaving a need for rapid, clinically applicable microbial detection methods.
- Infection prevention integration: Understanding where contamination risk occurs and how to rapidly detect it is essential for enhancing clinical safety protocols in regenerative therapy.
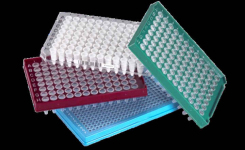
Key Findings: Assessment of microbial contamination risks during Platelet-Rich Plasma preparation and suitable rapid microbial detection methods revealed the following findings1:
Contamination Risk Across PRP Workflow
- Venipuncture contamination: After standard skin disinfection, microbial colonies were still detected at the venipuncture site in 60% if patients, including Bacillus subtilis and Micrococcus spp.
- Preparation environment contamination: Environmental monitoring at 3 PRP preparation sites showed airborne microbes; areas without pressure control had higher colony counts than those with clean-room conditions. Common environmental and skin bacteria were identified in preparation areas, including Micrococcus spp., Staphylococcus aureus, and Streptococcus spp., with counts influenced by clean-bench usage and room traffic.
- Sterility of final PRP: Standard sterility cultures on 85 PRP samples were negative, but the sample size was likely too small to elaborate true contamination rates.
Rapid Microbial Detection Methods
- Flow cytometry (FCM): Effective and efficient at detecting viable bacteria at ~10² - 10³ cfu/mL in PRP, though it failed to distinguish Candida albicans from PRP background signals.
- Polymerase chain reaction (PCR): Yielded false negatives and false positives when used on PRP samples, likely due to extraction/amplification interference from PRP components.
- Traditional sterility tests: These remained more sensitive overall but are too slow for point-of-care PRP assessment.
Bigger Picture: This study by Arita et al. highlights that microbial contamination risks exist at multiple steps in the PRP therapy process—particularly during venipuncture and preparation—even when standard disinfection is used. Rapid microbial detection methods, such as flow cytometry, show promise for clinical application, offering faster detection of viable organisms than traditional culture methods. However, further optimisation is needed for fungal and low-level contaminants. PCR, while sensitive in controlled settings, is limited by interference from PRP components. Clinicians providing PRP therapy should incorporate rigorous aseptic techniques, facility-specific contamination controls, and consider implementing rapid detection protocols where feasible. These measures are essential to mitigate infection risk and ensure patient safety as the use of PRP therapy expands.
(Image Credit: iStock/ 1933bkk)
References:
- Arita et al. 2026. Microbial Contamination Risks and Clinical Safety in Platelet-Rich Plasma Therapy and Evaluation of Rapid Microbial Detection Methods. Regenerative Therapy.