NOTE: If health care providers suspect a possible case of monkeypox, immediately contact your county health department or the 24/7 disease reporting hotline at (850) 245-4401. Local county health departments can help providers obtain monkeypox virus-specific real-time polymerase chain reaction (PCR) testing.
Monkeypox was first identified in the 1950s but, until recently, it has remained relatively rare. As healthcare providers now face an increased likelihood of coming into contact with this disease, it’s important to have best practices in place for testing. A key element of testing accuracy is the use of the most effective diagnostic tools for specimen collection and testing.
In this article, we’ll provide background for identifying monkeypox, as well as guidance on the most effective practices for testing and specimen storage and transportation.
What is monkeypox?
Monkeypox is caused by infection with the monkeypox virus, a part of the same family of viruses as smallpox. In fact, its symptoms are similar to smallpox symptoms but milder and rarely fatal.
According to the Centers for Disease Control and Prevention (CDC), symptoms of monkeypox include:
- Fever
- Headache
- Muscle aches and backache
- Swollen lymph nodes
- Chills
- Exhaustion
- A rash that can look like pimples or blisters that appear on the face, inside the mouth, and on other parts of the body. In some cases, the rash may precede other symptoms while others may experience only a rash.
How monkeypox is spread
Anyone can catch monkeypox if they have close contact with someone infected with the virus. The CDC explains that while the monkeypox virus is not easily spread, it can be passed from an infected animal, infected person, or materials contaminated with the virus. The virus spreads through direct contact with an infected person’s body fluids or lesions or materials that have touched body fluids or lesions, such as clothing or linens. It also can be spread through respiratory secretions during prolonged, face-to-face contact.
Individuals who believe they have come into contact with someone infected by the monkeypox virus should pursue testing. Health care providers that suspect a case of monkeypox should contact their county health department to obtain monkeypox virus-specific real-time polymerase chain reaction (PCR) testing and to report the occurrence.
How do you test for monkeypox?
Testing for monkeypox is done using real-time PCR testing on lesion material. Specimens are collected by vigorously swabbing or brushing an infected lesion with a sterile dry swab. The CDC advises collecting multiple specimens for preliminary and confirmatory testing.
Because of the contagious nature of the virus, the subject should be isolated and the healthcare provider should wear personal protective equipment (PPE) in accordance with recommendations for healthcare settings.
How to prepare and collect monkeypox specimens
The CDC requests that healthcare professionals report possible human cases of monkeypox to their epidemiologist and/or infection control personnel, who will in turn report to your state’s health department. This consultation with the state health department and CDC should be done prior to collecting specimens.
Testing for monkeypox
If the individual being tested for monkeypox has an active lesion or rash, a specimen should be collected from the lesion material. A dry swab of lesion fluid or the surface of the lesion is acceptable.
- Don PPE, including a gown, gloves, eye protection, and a NIOSH-approved particulate respirator equipped with N95 filters or higher.
- Vigorously swab or brush the infected lesion with two separate dry, sterile swabs.
- Break off the tip end of each swab into a 1.5 - or 2-mL screw-capped tube or place each entire swab in a separate sterile container or into a viral transport media or universal transport media in a plastic vial.
The UK Health Security Agency recommends, For high-risk contacts of a confirmed case who have developed systemic symptoms but does not have a rash or lesions for sampling, you should take a throat swab in viral transport media.” For more information on how to collect a throat swab specimen, download our free infographic here.
Note that even if the throat swab is negative, the individual must continue with monitoring and isolation as instructed, and should be reassessed and sampled if further symptoms develop.
Storing and sending a monkeypox sample
The CDC strongly recommends freezing specimens within an hour of collection at -20°C or lower. If frozen, samples can be stored for up to 60 days. If no freezer is available, CDC recommends refrigerating samples at 2°C to 8°C within an hour of collection and storing them for up to seven days.
Swabs are transported to the state lab for a presumptive test. If the test is positive, the second collected swab will be sent to the CDC for confirmation of a positive case of monkeypox.
The best diagnostic products for monkeypox
Using appropriate diagnostic materials will help ensure accuracy in testing results. Below are a few of the materials recommended to collect the maximum amount of viral material for testing and maintain sample integrity until it can be tested.
Swabs
Any swab type can be used to collect specimens for monkeypox testing, except for cotton swabs. Cotton’s absorbent fiber does not allow for the efficient release of the collected specimen. And, of equal importance, its naturally occurring fatty acids may interfere with processes employed in microbiology and in DNA extraction.
Instead, healthcare providers may use rayon or spun polyester swabs with rigid plastic, wood or aluminum handles. Or healthcare providers may opt for flocked swabs to assure optimal specimen collection and release and greater patient comfort.
Puritan’s PurFlock Ultra® and HydraFlock® flock swabs utilize multi-length polyester fibers for superior collection and release properties when compared to standard nylon flock swabs. To achieve an even greater surface area for collection, the HydraFlock swab features split-end fibers that yield reliable results even with a minimum sample size.
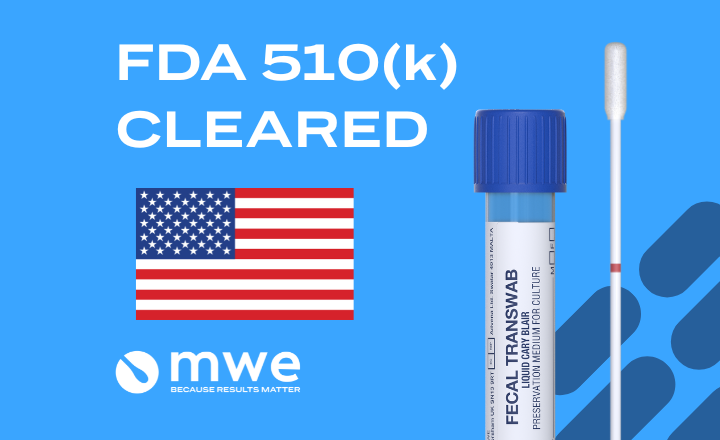
Transport tube
Transport tubes maintain sample integrity during transport for testing. The CDC recommends using plastic rather than glass materials for specimen collection, when possible to prevent accidental breakage.
Puritan uses virgin polypropylene resin for its dry transport system tubes to ensure a safe and sterile environment for swabs. An injection molded cap provides a precision fit and eliminates the risk of a foreign adhesive interfering with the specimen.
Tube labeling should display the product expiry date and provide room for patient identification and collection information. In some cases, labels may serve as a tamper-resistant seal between the tube and its cap.
Viral transport medium
While the use of viral or universal transport medium is not required, the use of this solution will allow maximum DNA collection and the least dilution. This liquid provides a balanced buffer solution to maintain a neutral pH, as well as antimicrobial agents, protein sources, and sucrose to preserve the sample during storage and transport.
Find the right combination of tools
Codes for Puritan's sterile swabs in dry transport tubes include the following:25-3206-U/H 20MM BT (Sterile elongated flock swab with a plastic handle and dry transport tube)
25-3406-U/H BT (Large flock-tipped applicator with polystyrene handle in dry transport tube)
25-3606-U/H BT (Elongated flock-tipped applicator with polystyrene handle in dry transport tube)
25-3706-U/H BT (Elongated flock-tipped applicator with polystyrene handle in dry transport tube)
25-3806-U/H BT (Elongated flock-tipped applicator with polystyrene handle in dry transport tube)
UT-100 (Vial filled with 1ml universal transport medium)
UT-300 (Vial filled with 3ml universal transport medium)
UT-106 (1ml universal transport medium filled vial and one large tipped PurFlock Ultra® applicator)
UT-306 (3ml universal transport medium filled vial and one elongated PurFlock Ultra® applicator)
UT-361 (3ml universal transport medium filled vial and one standard polyester swab)
VL 1201 SAFE (1 ml DNA/RNA preservative filled in a polypropylene screw-cap vial)
VL 1201 SAFE-H (1ml DNA/RNA preservative in a light blue polypropylene screw-cap vial with a large HydraFlock swab)
To learn more about the types of diagnostic tools available for accurate testing, click here or contact the supplier for more details using the green "Request Information" button below