Protecting Women&rsq...
6th October 2021 Content supplied by: Jiangsu Bioperfectus Technologies Co., Ltd.
The Devil in the Details - Contamination in a PCR Lab
Using Real-time PCR to detect SARS-CoV-2 has the advantage of high sensitivity and specificity, making it the "gold standard" for COVID-19 diagnosis. However, its capacity to produce millions of copies from just a few initial copies of a specific target brings with it a headache for molecular technicians: the contamination issue.
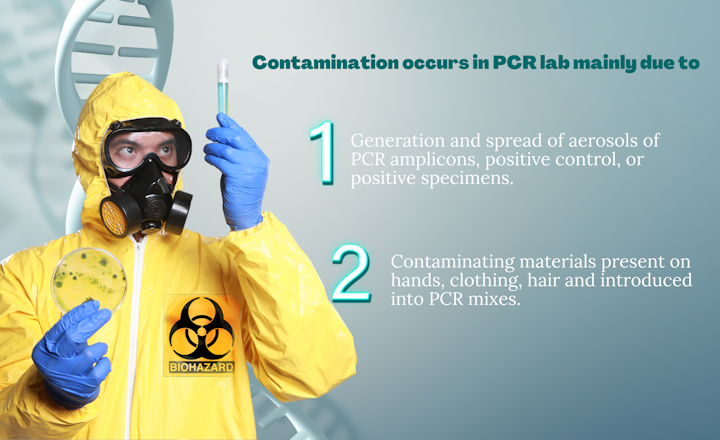
Primary reasons for contamination during PCR:
- Generation and spread of aerosols of PCR amplicons, positive control, or positive specimens.
- Contamination introduced to PCR mixes from hands, clothes, and hair.
These contamination issues can result in false-positive results, and moreover, it's very hard to be reduced or removed once it has occurred. Therefore, the prevention of contamination plays a much more important role in a PCR Lab. Proper laboratory setup and workflow, together with Good Laboratory Practice (GLP), will greatly help to reduce the likelihood of contamination.
In this article, we've (Bioperfectus) summarized some tips for setting up a PCR lab and included basic practices and procedures for avoiding contamination.
PCR Laboratory Set-Up
Physical separation of work areas
A laboratory performing PCR analyses on diagnostic samples should be divided into at least three physically separate rooms (Fig 1.)
- Reagent preparation area
- Sample preparation area
- Amplification and product detection area
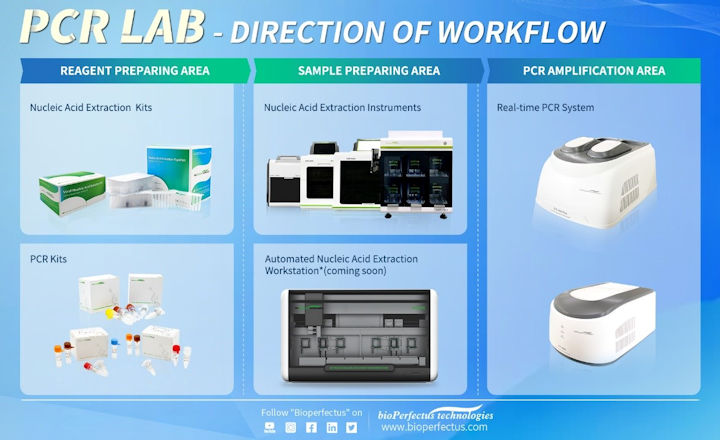
Fig 1. Three separate areas are required for PCR analyses.
The reagent preparation area is for reagent aliquoting and master-mix preparation. This room should be the cleanest of all spaces used to prepare PCR experiments and should ideally be in a designated laminar flow cabinet equipped with a UV light. PCR reagents should be kept in a refrigerator (per manufacturer's recommendations) in the same designated area, ideally next to the laminar flow cabinet. The Master-mix should be prepared and aliquoted in the reaction vessel, and extracted nucleic acid and amplified PCR products must not be handled in this area.
The sample preparation area is for nucleic acid extraction and DNA template and controls addition. Ideally, samples should be added in a designated biosafety cabinet equipped with a UV light. To avoid contamination of the extracted nucleic acid samples analyzed, it is recommended to first add sample and negative control, then lastly add positive controls or standards. Samples should be stored in designated fridges and freezers in the same area, but PCR reagents and amplified products must not be pipetted in this area.
The amplification and product detection area is for amplification and handling of amplified products and product analysis (not for real-time PCR). It usually contains thermocyclers and real-time platforms. Ideally, a laminar flow cabinet would be used for any steps that require manipulating open tubes after PCR amplification.
Air pressure and air conditioning:
- Reagent preparation area (using positive air pressure to prevent the introduction of contamination)
- Sample preparation area (using negative air pressure to keep template nucleic acids in the room)
- Amplification and product detection area (using negative pressure to keep amplified nucleic acids in the room)
- The air handlers for the three areas need to be connected to separate air ducts, and each must lead to a separate location for exhaust. Do NOT use central air-conditioning system and ductwork for the three areas.
Unidirectional workflow
When a PCR procedure starts, the direction will be Reagent Preparing Area → Sample Preparing Area → PCR Amplification Area. NEVER return previously processed tubes to the preceding work area or room. Operators who have worked in post-PCR should not go back and work in pre-PCR. Also, the consumables and PPE (lab coats, gloves, goggles, etc.) that have been introduced into the post-PCR room should never be placed back in the pre-PCR room without thorough decontamination. Waste materials that contain PCR amplicons should not be allowed to accumulate in an area close to the personnel involved with template isolation and purification.
Dedicated equipment and consumables
Besides the separated spaces, all the supplies and equipment such as centrifuges, storage freezers/refrigerators, pipettors, reagents, pipettor tips, racks, and so forth should be dedicated to each area and should not be interchanged between areas. Also, the lab coats for the operator should be dedicated to three areas separately.
PCR Laboratory Operation
Surface and equipment decontamination
By using 70% ethanol to clean work surfaces and equipment before and after, contamination can be reduced. Regularly use a freshly made 10–15% sodium hypochlorite to clean the surface and wait 10 to 15 minutes before wiping down with de-ionized water. Alternatively, commercially available products that are validated as DNA-destroying surface decontaminants can be used if sodium hypochlorite is not suitable for decontaminating the metallic parts of equipment. If using 70% ethanol instead of sodium hypochlorite, irradiation with UV light will be needed to complete the decontamination.
UV light
Before use, the laminar flow cabinet or biosafety cabinet should be decontaminated using a UV light for at least half an hour and cleaned with 70% ethanol. The airflow and HEPA filtration in all hoods should be monitored and certified as per manufacturers' recommendations. Regularly expose the working areas and room to UV light overnight.
Using aerosol barrier tips
Aerosols can lead to cross-contamination from sample to sample. Aerosol barrier pipette tips could prevent the reintroduction of small amounts of a contaminating aerosolized sample into the next sample that is pipetted. In addition, a correct pipetting technique also helps to reduce contamination. Incorrect pipetting may result in splashing when dispensing liquids and the creation of aerosols.
Carefully open and close sample tubes
All sample tubes and reaction plates should be opened and closed very carefully to make sure the liquid doesn't splash out. Spinning tubes/plates before opening can prevent aerosols when opening.
Setup controls on every PCR experiment
Include well-characterized, confirmed positive and negative controls, along with a no-template control (NTC) in all reactions. The positive control should not be in very high concentration as it poses a contamination risk. An NTC is used to check for the absence of contamination in the reagents, consumables, and environment.
Uracil-DNA-glycosylase (UDG) / uracil-N-glycosylase (UNG)
The use of UDG/UNG and dUTP substituted for dTTP could help to remove carryover amplification contamination from the previous PCR reactions. The UDG/UNG method works best with T-rich amplification products and is not as effective with GC-rich amplification products. UDG/UNG is not effective for sources of DNA contamination, other than dUTP-containing amplification products from previous qPCR experiments.
Conclusion
This article listed several common approaches to reduce or avoid contamination in the PCR laboratory for your reference. You may refer to the above tips and combine them with your local guidance and good laboratory practice to prevent the occurrence of contamination.
Bioperfectus provides a total solution to the PCR laboratory. Contact us today by using the 'Request Information' button provided below the references or visit Bioperfectus.com to learn more.
References:
1. Establishment of PCR laboratory in developing countries, 2nd edition. The World Health Organization.
2. Dos and Don'ts for molecular testing. The World Health Organization: Global Malaria programme.
3. Setting up a PCR Laboratory. Mifflin TE. CSH Protoc. 2007 Jul 1; 2007: pdb. top14. doi: 10.1101/pdb. top 14. PMID: 21357132.
4. The Polymerase chain reaction. Ausubel FM. In: Ausubel F, Brent R, Moore D, Seidman JG, Smith J, Struhl K, editors. Current Protocols in Molecular Biology, John Wiley & Sons, Inc., U.S.A., Vol. 2, Chapter 15, 1999; 15.01
5. Preventing PCR amplification carryover contamination in a clinical laboratory. Aslanzadeh J (2004). Ann Clin Lab Sci 34(4):389–96
Tags:
Date Published: 6th October 2021
Source article link: View
Protecting Women’s Health &